Patient History: A 24-year-old male student presents with a 2-month history of progressive dyspnea (shortness of breath) on exertion and when lying on his right side and a persistent, dry cough. He denies any fever, night sweats, or unintentional weight loss.
Examination Findings:
Vitals: HR: 90 bpm, O2 Sat: 94% on room air, Temp: 37.0°C.
Resp: Trachea deviated towards right side.
Decreased breath sounds and significant dullness (stony dullness) to percussion over the entire left lung field.
Vocal fremitus and vocal resonance are absent on left side.
Lymph: No peripheral lymphadenopathy is palpable.
You correctly order a Chest X-ray.
Investigation Findings:
CXR Report: Large, opacified left hemithorax consistent with a large pleural effusion. There is a contralateral mediastinal shift. The upper mediastinum appears widened.
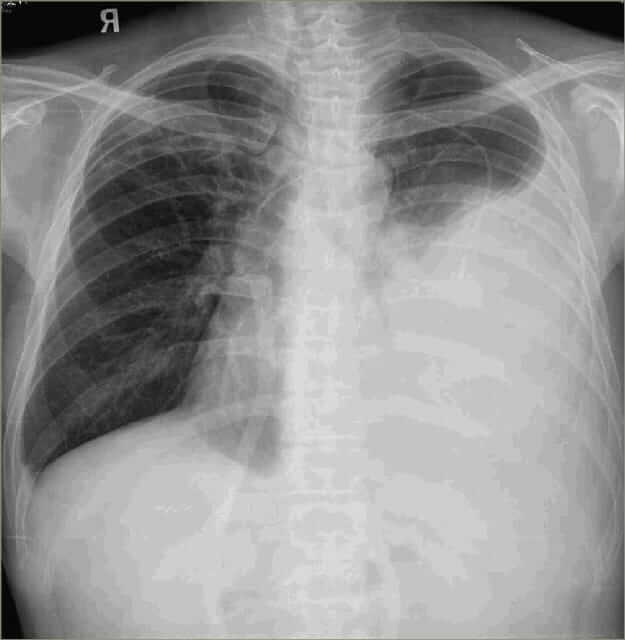
No improvement in dyspnea, patient worsens. Your senior explains there was nothing pointing towards infection and you should have evaluated further. He orders Chest X-ray.
CXR Report: Large, opacified left hemithorax consistent with large pleural effusion. Contralateral mediastinal shift. Upper mediastinum appears widened.
Patient returns with ECG showing decreased voltage in V4-V6, right axis deviation. Findings inconclusive for cardiac etiology. Your senior asks for Chest X-ray.
CXR Report: Large, opacified left hemithorax consistent with large pleural effusion. Contralateral mediastinal shift. Upper mediastinum widened.
No improvement in dyspnea, patient worsens. Your senior explains nothing pointed towards obstructive lung disease and you should have evaluated further. Chest X-ray ordered.
CXR Report: Large, opacified left hemithorax consistent with large pleural effusion. Contralateral mediastinal shift. Upper mediastinum widened.
You prepare for thoracentesis.
Finding: You drain 1.5 liters of thick, milky-white, odorless fluid. Patient’s breathing improves immediately.
Patient’s dyspnea worsens with diuretics. Your senior explains diuretics only help transudative effusions from systemic fluid overload.
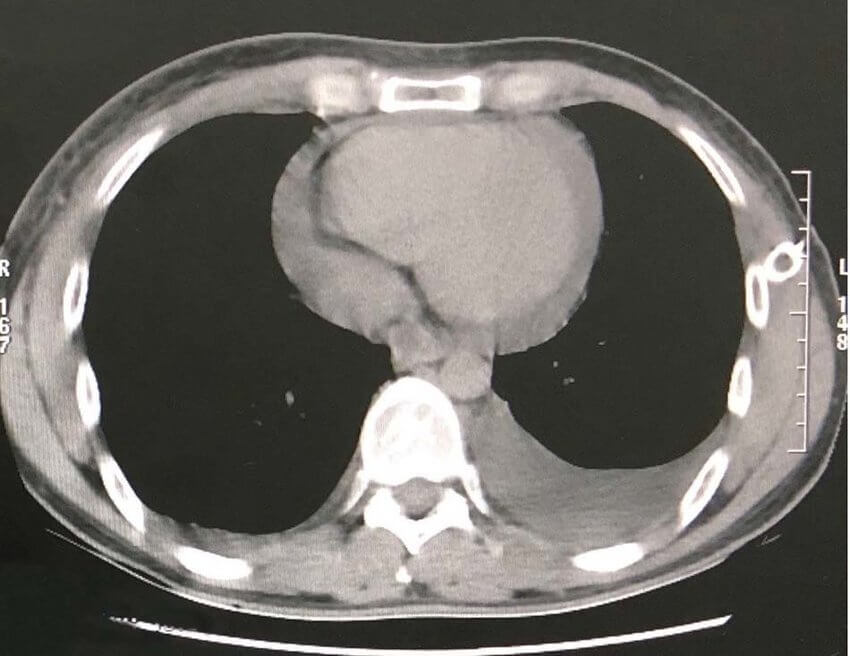
CT shows large 10cm anterior mediastinal mass. Patient’s O2 saturation falls to 89%. Your consultant asks you to manage.
A series of critical errors occurred. The cardinal physical exam finding (unilateral stony dullness) and the 2-month timeline were not appropriately addressed, leading to significant delay in diagnosing a life-threatening but curable condition.
You scored 0 points.
Thank you for completing the case!
Emergency chest tube inserted. 2L of thick milky-white fluid drained. Patient improved slightly. Tube draining 1L/day.
Lab findings: Triglycerides: 510mg/dL
Pleural Fluid Analysis:
Gross: Milky-white
Triglycerides: 510 mg/dL, Cholesterol: 80 mg/dL
Chylomicrons: Present
Cell Count: 2500 cells/uL (95% Lymphocytes)
Cytology: Atypical large lymphoid cells present
Exudate by Light’s criteria
You start IV antibiotics. 48 hours pass - no growth on cultures. Your senior says your diagnosis is wrong.
Correct diagnosis made after significant delays. Patient subjected to prolonged chest tube drainage leading to severe malnutrition and immunologic incompetence, complicating upcoming chemotherapy.
Feedback: Key difference: Cholesterol/TG ratio >1 in Pseudochylothorax, <1 in Chylothorax. Cholesterol crystals pathognomonic for Pseudochylothorax.
You scored 0 points.
Thank you for completing the case!
Confirmed exudative Chylothorax due to likely malignancy. CECT shows large 10cm anterior mediastinal mass.
You start supportive treatment but haven’t investigated the cause. Patient stable but not cured.
Diagnosis made after significant delays. Prolonged chest tube drainage led to severe malnutrition and immunologic incompetence.
Feedback: Most common chylothorax causes: traumatic and non-traumatic. Without trauma, mediastinal malignancy top differential - should be evaluated with biopsy.
You scored 0 points.
Thank you for completing the case!
Pathology Report:
H&E: Effacement of lymph node architecture by fibrosis. Mixed cellular infiltrate. Large, atypical, bi-nucleated cells with prominent eosinophilic nucleoli.
IHC: CD30+, CD15+, weakly PAX5+, CD20-, CD45-.
Perfect! You correctly identified Reed-Sternberg cells and CD30+/CD15+ immunophenotype as Nodular Sclerosis Hodgkin’s Lymphoma. Selected correct ABVD chemotherapy.
Chylothorax resolved after first cycle of chemo. Best possible outcome!
You scored 0 points.
Thank you for completing the case!
You identified need for biopsy but mis-identified pathology or selected wrong treatment.
Feedback: Findings specific for Hodgkin’s (CD15+/CD30+), not NHL or TB. Multi-agent chemotherapy (ABVD) is standard for bulky mediastinal Hodgkin’s. Error delay correct treatment but diagnosis now established.
You scored 0 points.
Thank you for completing the case!