A 67-year-old man is brought to casualty after suddenly developing slurred speech and right-sided weakness 1 hour ago. He was previously normal.
History: Hypertension, type 2 diabetes mellitus, hyperlipidemia
Medications: Amlodipine, metformin, atorvastatin
Vitals: BP 168/94 mmHg, HR 92/min, RR 18/min, SpO₂ 96% RA
Neurological exam: Slurred speech, right facial droop, right arm/leg weakness, decreased pinprick sensation right arm
Your fellow resident stops you: ‘Where are you taking him? We don’t have glucose level yet. It might be hypoglycemia.’
Reassessment: Airway intact, breathing no distress, circulation stable, glucose 108 mg/dL
Vitals unchanged: BP 168/94, HR 92, RR 18, SpO₂ 96%
Initial assessment complete:
Airway intact, breathing no distress, circulation stable, glucose 108 mg/dL
Vitals unchanged. You activate stroke protocol.
Nurse stops you: ‘No aspirin until we know it’s not a bleed.’ Senior resident steps in. You confirm ABCs stable and glucose 108 mg/dL.
Non-contrast CT head (20 min after arrival):
No intracranial hemorrhage, no mass effect
Subtle early ischemic changes in left MCA territory
Good ASPECTS score
You send patient for MRI but radiologist calls: ‘Cannot mobilize MRI early enough! Wasting time!’ Senior redirects you.
As you open aspirin, nurse stops you: ‘No antiplatelets until we know it’s not a bleed!’ Fellow resident: ‘Don’t stall, need imaging now!’
As you order IV labetalol to lower BP, fellow resident stops you: ‘Why lower pressure? If ischemic stroke, you’ll worsen perfusion!’ Patient unharmed but time lost.
You order CT angiogram as first imaging. Radiology calls: ‘Will take time… sure you want this as first-line?’ You realize mistake and cancel.
You order labs first. 12 minutes pass, neurological deficit worsened. Senior: ‘Imaging comes first in stroke. Labs do NOT delay imaging.’
Finish 1 — Critical Error
You gave clopidogrel before imaging. Patient becomes acutely drowsy, BP spikes, vomits, right pupil dilates.
CT shows large left intracerebral hemorrhage.
Clopidogrel worsened bleeding. Patient intubated, emergency decompression, remains critical.
You’re removed from the team.
You scored 0 points.
Thank you for completing the case!
CTA Results: Left M1 occlusion, no carotid dissection, no significant carotid stenosis, moderate collateral flow
Time since onset: ~1 hour 35 minutes
BP 170/96, glucose 108 mg/dL
No contraindications to thrombolysis
Nurse: ‘Should we thrombolyse?’
You realize aspirin can’t reopen blocked artery. Need to assess thrombolysis eligibility first.
Time since onset: ~1 hour 35 minutes
BP 168/94, glucose 108 mg/dL
No contraindications
Assessing for IV thrombolysis:
Time since onset: ~1 hour 35 minutes
NCCT: no hemorrhage
BP 168/94, glucose 108 mg/dL
No contraindications, good ASPECTS
You order CTA but realize mistake, order NCCT instead.
NCCT Findings: No hemorrhage, subtle early ischemic changes left MCA, good ASPECTS
You initiate IV alteplase. Bolus given, infusion running smoothly. Resident: ‘Good. Now what? Alteplase alone might not suffice for LVO.’
You lower BP before thrombolysis, then realize BP doesn’t need to be this low - tPA only requires <185/110 mmHg.
You prioritize mechanical thrombectomy for M1 occlusion. IR team: ‘Giving IV thrombolysis first? We can do drip-and-ship.’
You skip thrombolysis due to hemorrhage risk. Senior: ‘Inside 4.5-hour window, no contraindications, good ASPECTS. Can’t deny reperfusion!’
You proceed with IV alteplase. CTA shows proximal left M1 occlusion.
Senior: ‘Alteplase alone has limited efficacy in LVO.’
You lower BP before reperfusion, then realize mistake - tPA only requires <185/110 mmHg.
You prioritize thrombectomy but realize guidelines require thrombolysis first. You give alteplase. CTA shows M1 occlusion.
Senior: ‘Alteplase alone limited in LVO.’
You skip thrombolysis due to hemorrhage risk. Senior: ‘Inside 4.5-hour window, no contraindications. Can’t deny reperfusion!’
You prescribe aspirin + clopidogrel. Resident: ‘Antiplatelets don’t recanalize M1 clot, increase hemorrhage risk after alteplase!’
You try to repeat CTA. Resident: ‘Why waste time? We know there’s LVO - that’s why thrombectomy exists!’
Thrombectomy successful: Clot retrieved from left M1, complete flow restoration
Speech improving, right-sided weakness improving
No hemorrhagic transformation
Senior: ‘Great job! Now figure out why he had stroke to prevent next one.’
Thrombectomy successful: Clot retrieved from left M1, complete flow restoration
Speech improving, right-sided weakness improving
No hemorrhagic transformation
Senior: ‘Great job! Now figure out why he had stroke to prevent next one.’
You initiate IV alteplase and notify IR for ‘drip-and-ship’
Thrombectomy successful: Clot retrieved from left M1, complete flow restoration
Speech improving, right-sided weakness improving
No hemorrhagic transformation
Senior: ‘Great job! Now figure out why he had stroke to prevent next one.’
IR team: ‘Patient has no contraindications. Drip-and-ship improves outcomes even with LVO.’ You admit mistake and give alteplase.
Thrombectomy successful: Clot retrieved from left M1, complete flow restoration
Speech improving, right-sided weakness improving
No hemorrhagic transformation
Senior: ‘Great job! Now figure out why he had stroke to prevent next one.’
You lower BP before reperfusion, then realize mistake - tPA only requires <185/110 mmHg, current BP 168/94.
You wait to see if alteplase works alone. Senior: ‘Why waiting? LVO rarely recanalizes with alteplase alone!’
You stop alteplase for thrombectomy. IR informs you: ‘Wasn’t necessary - keep infusion running during transfer.’ You restart.
Thrombectomy successful: Clot retrieved from left M1, complete flow restoration
Speech improving, right-sided weakness improving
No hemorrhagic transformation
Senior: ‘Great job! Now figure out why he had stroke to prevent next one.’
You lower BP before reperfusion, then realize mistake - tPA only requires <185/110 mmHg.
You start dual antiplatelet therapy. Senior: ‘That was major LVO! Can’t just wait for OPD workup! Patient could be back tomorrow!’
Morning after thrombectomy: Speech clearer, right-sided power 4+/5
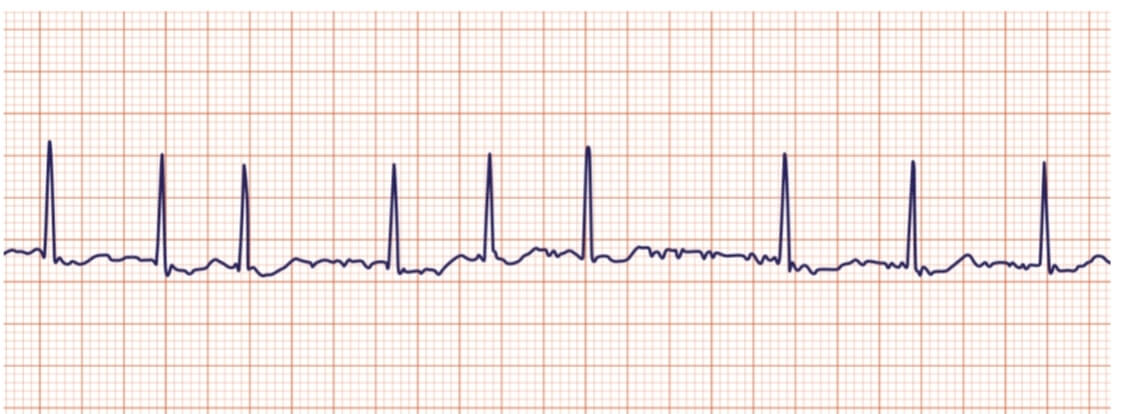
Cardiac monitoring: Episode of atrial fibrillation lasting 40 seconds
Echo: No structural heart disease, normal LV function, no thrombus, bubble study negative
You order hypercoagulability tests. Senior: ‘67-year-old with HTN, DM, hyperlipidemia - common stroke reasons! Rule out common causes first.’
Finish 2 — Fatal Error
You start heparin before new CT. Patient becomes drowsy, unequal pupils.
CT shows large intraparenchymal hemorrhage with mass effect and brain herniation.
Patient deteriorates rapidly, arrests. Resuscitation unsuccessful.
Removed from team.
You scored 0 points.
Thank you for completing the case!
Repeat head CT (24h post-thrombectomy): No hemorrhagic transformation
Senior: ‘Good. Now start secondary prevention for AF-related cardioembolic stroke.’
Patient alert, improving, BP 138/84, glucose controlled
No contraindications to anticoagulation
Finish 3 — Fatal Error
You start anticoagulation immediately. Patient becomes drowsy, GCS drops to 10.
CT shows large left-sided intracerebral hemorrhage with mass effect.
Initial scan only ruled out procedural bleeding - delayed hemorrhagic transformation risk.
Anticoagulation accelerated hemorrhage. Neurosurgery called but hemorrhage massive.
Patient deteriorates into herniation, pronounced dead.
You scored 0 points.
Thank you for completing the case!
You order prolonged Holter monitoring. Senior: ‘We already have documented paroxysmal AF. Don’t need more evidence.’
Senior: ‘Hypercoag tests waste money and delay diagnosis. For patient with risk factors, not required!’
Cardiac monitoring: Episode of atrial fibrillation
Echo: No structural heart disease, normal LV function, no thrombus

You start apixaban 5 mg twice daily for AF-related cardioembolic stroke.
Patient improving steadily, neurologically stable, BP controlled, ready for discharge.
Senior: ‘Good work! Finalize secondary prevention - lifelong anticoagulation, aggressive risk-factor control.’
Which discharge plan most appropriate?
You decide to start aspirin and clopidogrel instead of anticoagulation, but your senior immediately stops you.
‘This is a cardioembolic stroke from atrial fibrillation. AF doesn’t form platelet-rich clots like the ones seen in arteries, it forms fibrin-rich, coagulation-driven thrombi inside the left atrium!’ He cancels the order and waits for your corrected decision.
You decide to wait another 2-3 days before starting anticoagulation and continue aspirin alone to be safe. Your senior immediately corrects you.
‘Why are you waiting? We already have a 24-hour CT showing no hemorrhage. This is the exact moment to begin anticoagulation. The longer you delay, the more you risk a recurrent stroke!’
You start the patient on apixaban, 5 mg twice daily for AF-related cardioembolic stroke, and discontinue aspirin. His condition is improving steadily. He’s neurologically stable, BP is controlled, and he’s medically ready for discharge planning.
Senior: ‘Good work! Finalize secondary prevention - lifelong anticoagulation, and aggressive risk-factor control.’
Which discharge plan most appropriate?
Finish 4 — Perfect Outcome
Discharge plan perfect: anticoagulation for AF, high-intensity statins, BP control, diabetes management, rehab.
Senior presents your orders to team: ‘This is exactly how secondary prevention should look!’
Patient’s gait improving, proper counseling for long-term adherence.
Discharged home with family support and clear follow-up.
You scored 0 points.
Thank you for completing the case!
Finish 5 — Good but Flawed
Senior pauses at DAPT: ‘With atrial fibrillation, anticoagulation alone is treatment. Adding aspirin+clopidogrel increases bleeding risk - GI, intracranial, no benefit.’
Deletes DAPT before discharge.
Overall management decent but introduced unnecessary hazard.
Patient improves rapidly, discharged home safely.
You scored 0 points.
Thank you for completing the case!
Finish 6 — Good but Incomplete
Senior: ‘Medications fine but skipped rehab. After MCA stroke, need structured physiotherapy, gait training, speech therapy to prevent long-term disability.’
Adds rehab referrals.
Patient remains stable, discharged safely but plan lacked key pillar of post-stroke care.
You scored 0 points.
Thank you for completing the case!